A personal experience and things you should know about spinal fusion surgery

My husband and I weren’t surprised – but were still filled with dread – when an orthopedic surgeon told us it was time to seriously consider spinal fusion surgery for our daughter. At the time our daughter, Jilly, was 12 years old and had been followed by the surgeon since she was 3, seeing him one or two times per year. As a young person with Rett syndrome, we knew her chances of spinal surgery were high because weak muscles and limited mobility typically lead to severe scoliosis. Although the progression was slow and we did everything in our power to fight it, including physical therapy and bracing her spine, we were unable to avoid the inevitable: a curving of Jilly’s spine that began to crush her organs and prevented her from sitting up straight.
It’s important to remember that when it comes to any kind of surgical procedure, every person is different, and that there are multiple versions of spinal fusion. This experience was our family’s, and though yours will be different, I believe that sharing our story can bring some comfort to an otherwise difficult situation.
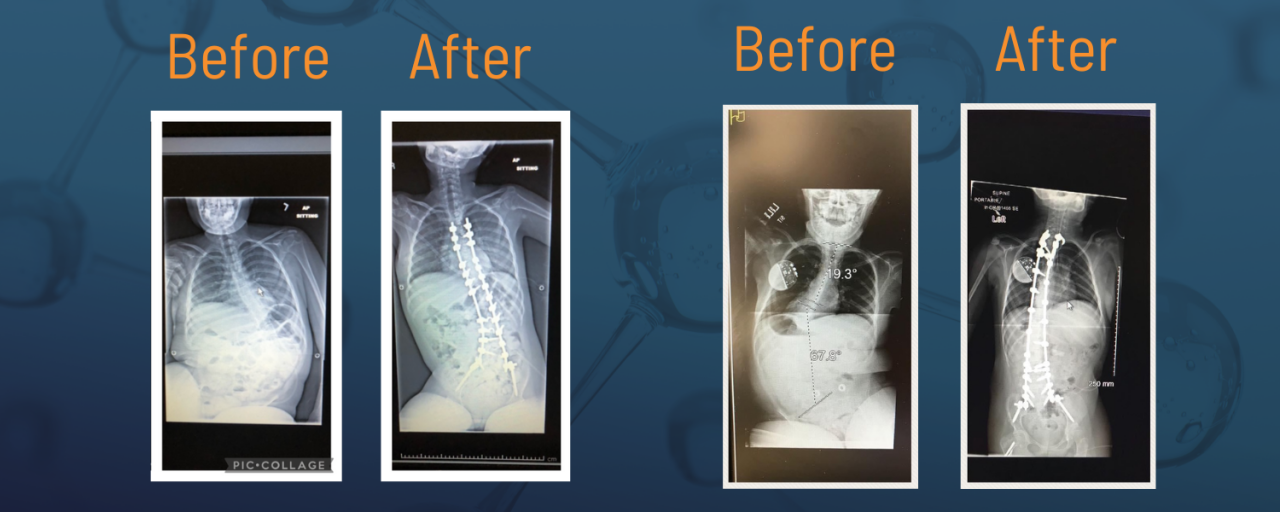
Jilly’s curve progressed slowly at first, but, in the year before surgery became imminent, her curve rapidly progressed. It began to impact her respiratory and GI systems and significantly affect her quality of life. She began to vomit frequently, aspirate, and then get pneumonia. This turned into a vicious cycle that led to several hospitalizations. In addition, Jilly was so hunched over to her right side that she required constant propping with pillows and blankets just so she could be somewhat upright. It became difficult for her to participate in what was going on around her because it was nearly impossible for her to lift her head as a result of the curve.
Because of her pneumonia and hospitalizations, Jilly wasn’t healthy enough for surgery until a couple of years after that first conversation. At age 14 there finally came a window when doctors felt confident that she’d be able to get through it.
The weeks and days leading up to her surgery in January of 2017 were brutal. I was consumed with fear, anxiety, and apprehension. I tried to stay positive and hopeful, but it was impossible not to imagine the worst because spinal fusion is considered a major surgery and has a high risk of complications.
The night before surgery was one of the hardest experiences of our lives, but I am happy to report that once we arrived at the hospital for pre-op, a sense of calm came over us. My husband and I felt ready to get the surgery underway, and couldn’t wait to see our brave girl later that day. In the weeks leading up to the surgery we had talked to Jilly at a superficial level about what was going to happen, not sharing too many details but explaining how much better she’d be feeling after it was done. We also talked with many families who had already gone through the surgery, and their feedback was similar: Their children were living better lives because of the spinal fusion, they were healthier and happier. We recalled these conversations as we waited nervously for Jilly’s surgery to end, and they truly helped us get through the day.
For example, Oakley had spinal surgery when she was 12. Oakley’s mom, Shannon, describes her today, at 13, as so much more alert and confident. Shannon says Oakley’s stamina is better when it comes to sitting, eating, and staying awake. The surgery also helped with Oakley’s reflux and some of her digestion issues.
But the feelings you experience leading up to surgery can be excruciating. Brooklyn, who is now 17, had spinal surgery when she was 12. Her mother, Kelly, remembers how heightened her emotions were leading up to the surgery. “Although I was a seasoned ‘Rett mama’ by the time of Brooklyn’s surgery, my fear and anxiety were at an all-time high leading up to surgery day,” Kelly shared. “Honestly, though, I can thankfully say all of those emotions were WAY worse than the actual surgery and recovery experience.”

Jilly’s surgery lasted about seven hours. She spent about 36 hours in the PICU at Boston Children’s Hospital afterward, where she was carefully monitored. Within just a few hours she was taken off the ventilator, which she had been on during the surgery. Her face was a bit swollen and quite pale, but overall she looked like our Jilly. It was the best feeling in the world to hold her hand and know she was okay.
In less than two days Jilly was discharged from the PICU and admitted to a different floor for recovery. I had heard it would be important to get her out of bed and into her chair quickly, but I was shocked to have her do so two days after surgery. In true Jilly fashion, she literally rose to the occasion and tolerated sitting. I will never forget the image of her sitting up so straight and so tall for the first time. She was able to make eye contact and, after so long, she was finally going to be able to be a part of what was going on around her, as well as be at less risk for illnesses and hospitalizations.
Jilly had a few complications on the road to recovery. It is impossible to predict or plan for these, and every person and surgery is different, so we dealt with each situation as it came. She was discharged one week after the initial surgery but unfortunately rehospitalized due to infection despite our diligent care. I have talked with many families who have daughters who experienced zero complications and who sailed right through the surgery; they were home within a week and back to school within just a couple of weeks. I cannot overemphasize that every journey with scoliosis surgery is unique.
Although the experience was intense and scary, we’d do it again in a heartbeat. Today, at age 19, Jilly sits tall and is more alert than she has ever been in her life. She has been pneumonia-free and stayed out of the hospital for more than five years. She is the happiest and giggliest we have ever seen her, and that is what makes us the most happy.
There are many things I wish I had known before embarking on this journey with Jilly. Here are things that come to mind that might help you if you are looking at spinal fusion surgery:
Tips for leading up to surgery:
- Discuss anesthesia options with your child's surgeon and decide what is best for your child.
- Create a plan for pain management; know what options are available.
- Discuss a plan for management of GI issues during and after surgery, such as constipation and/or diarrhea.
- If your child has a VNS, talk to your doctor about whether it will be kept on during surgery.
- Learn about blood transfusions in case your child needs one.
- Inquire about any medications that your child should take prior to surgery (stool softeners, antibiotics, etc.).
- Inquire about any medications your child should NOT take prior to surgery.
- Ask what the morning of/day of surgery will look like; ask what procedures and tests will be done prior to the surgery.
- Although it is helpful to talk to other parents, remember that every child is different and every child’s recovery is different.
Things to consider packing for the hospital:
- A pillow for your child and yourself.
- Blanket(s) for your child and yourself.
- Comfortable clothing, including warm socks and layers of clothing (hospital rooms can get chilly quickly).
- Slides, flip flops, or slippers with a rubber sole so that you can disinfect occasionally.
- Personal items and toiletries for yourself and your child, including lip balm, lotion, hair brush, etc. Rinse-free bath sponges helped when I wanted to clean Jilly on my own; I like the brand Scrubzz.
- Whatever devices you use for entertainment purposes. Don’t forget a charger!
- Consider making a playlist ahead of time of all your child’s favorite songs.
- Favorite DVD’s, although we had great movies on-demand.
- A notebook and pens. You will want to take notes on every conversation you have with every doctor during recovery. Even if you think you will remember, write it all down.
- Comforting objects that will bring joy to your child, such as a night light that displays colorful scenes on the ceiling, stuffed animals, etc.
- Leave all jewelry and valuable items at home.
Tips for when you’re in the hospital:
- Make sure physical therapy is occurring regularly; this is key to a faster and smoother recovery in general.
- Make sure respiratory therapy is also occurring regularly; this is key to keep the lungs clear. Inquire about using a positive airway pressure system.
- Keep in mind how important mobility within just a day or two after surgery is; attempt sitting up on the edge of the bed initially, then getting in a wheelchair, and, finally, walking (if your child walks).
- Massage your child’s feet and legs regularly; keep the circulation going.
- Allow your child plenty of rest, but, at the same time, be sure to stimulate her in order to get her to perk up and get back to baseline personality-wise; you and the clinicians will need to find the right balance.
Tips for after surgery:
- Prepare sleeping arrangements on the first floor of your home.
- Secure an adjustable/hospital bed; this is not mandatory but it’s helpful.
- Plan for how you will bathe your child once home; be sure to get detailed instructions on how to bathe her safely.
- Discuss how to prevent infection and maintain good hygiene; know what to look for infection-wise and know whom to call if something doesn’t look right.
- Inquire about supplements, such as collagen, that may help speed up the healing process.
- Make arrangements for respite and/or nursing assistance, especially for the first couple of weeks after returning home.
- Understand that a drain may be necessary for excessive fluids.
- Ask family and friends for help with day-to-day things like meals, grocery shopping, care for your other children, etc.
- Schedule, or at least know when to call to schedule, post-operative appointments.
- Learn how to best lift/transfer your child before you leave the hospital; be sure to practice this a few times before you are home.
- Ask for special instructions to share with your child’s PT, OT, nurse, teachers, etc.; she may not be able to do certain activities and exercises that she did prior to the surgery.
- Understand that recovery may take longer than anticipated; try to be patient.
If you are considering spinal fusion for your loved one and you want to correspond or talk to me about my experience, please don't hesitate to email me at jennifer@rsrt.org.
Kelly Butler and Shannon Madden contributed to this post.


